The risk of hemorrhage from traumatic injury exists in good times or bad, whether it’s due to a motor vehicle accident, a work mishap, civil unrest, or the zombie apocalypse. A major arterial bleed, if untreated, can cause a victim to be beyond medical help in just a few short minutes. The bleeding may be so severe that emergency medical personnel can’t arrive in time to help.
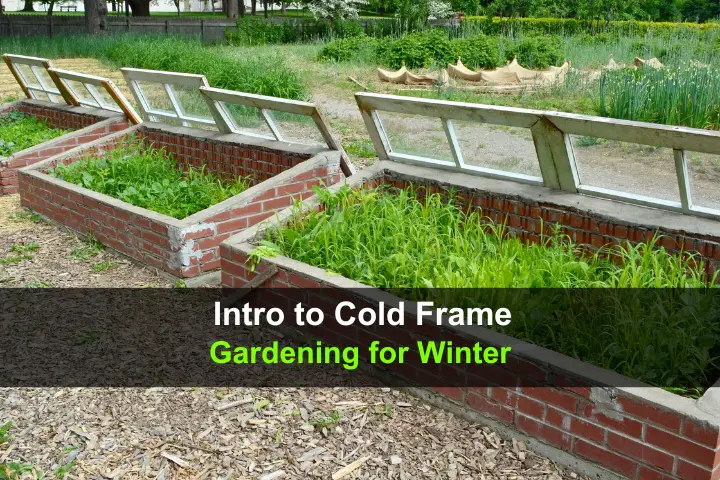
Having a way to control massive extremity bleeding is useful for the medic in survival settings. One of the most important tools for emergency hemorrhage control is the tourniquet. A tourniquet is a device that uses compression to stop the flow of blood through a vein or artery. Not having one in your medical kit can lead to a tragic outcome.
Here’s an example from our relatively recent past: After serving in the Texan and U.S. armies, Albert Sidney Johnston became a full general on the Confederate side in the Civil War. He was considered to be the best general they had at the time (Robert E. Lee had not yet ascended to command). At the battle of Shiloh in April 1862, General Johnston took a bullet behind the knee, severing a major artery. Unfortunately, no doctor was at hand and none on the battlefield thought to apply a tourniquet. It took an hour for him to bleed to death. Ironically, a tourniquet was later found in his pocket.
Even in recent conflicts, uncontrolled blood loss is a leading cause of fatality in potentially survivable battlefield injuries. The grand majority of these deaths occurred before the casualty was able to reach a modern medical facility. It’s imperative, therefore, for the effective medic in the field to have a working knowledge of bleeding wounds and the tools that staunch them.
ORIGINS OF TOURNIQUET USE
 Late 19th Century amputation set with tourniquet
Late 19th Century amputation set with tourniquet
Attempts to stop battlefield hemorrhage have been described in ancient writings as far back as the time of Alexander the Great. Usually, these efforts involved using a cloth or strap and a stick which was turned to apply pressure to a bleeding limb.
In the early 1700s, Jean Louis Petit, a French surgeon, developed a strap with a screw that could be turned to effectively compress blood vessels and stop bleeding. The word “tourniquet” developed from the French verb “tourner” (to turn). During the American Civil War, more than 50,000 strap tourniquets and 13,000 Petit screw tourniquets were employed on the Union side, mostly to facilitate the performance of more than 29,000 amputations.
Since then, the tourniquet has been both praised as a life-saver and vilified as a limb-loser. In the 21st century, our attitudes have turned towards the former: A 2013 study of the military’s experience in Iraq and Afghanistan showed that nearly a quarter of combat deaths due to hemorrhage between 2001 and 2011 might have been prevented with the right equipment and training. Therefore, every U.S. soldier now carries a tourniquet in an individual first aid kit (IFAK).
THE PHYSICAL EFFECTS OF BLEEDING
Although the amount of blood in the human body varies depending on sex, weight, age, and even altitude, an estimate of 9 to 10 pints is about average. How does blood loss affect what signs and symptoms a rescuer would note in a victim?
The American College of Surgeons identifies four classes of hemorrhage with their signs and symptoms:
Class I: 1.5 pints (0.75 liters) or less: little or no effect; you can donate a pint of whole blood, for example, as often as every 8 weeks. The victim may be somewhat anxious (after all, there’s blood). Pulse may rise a bit, but blood pressure and respirations are normal.
Class II: 1.5-3.0 pints (0.75-1.5 liters): The victim is usually agitated, with a rapid heartbeat (over 100 beats per minute) and respirations (20-30 per minute) as the body speeds up processes that allow the smaller population of red blood cells to deliver oxygen to tissues. Blood pressure remains within normal limits for now. The skin becomes cool and may appear pale.
Class III: 3.0-4 pints (1.5-2 liters): Blood pressure begins to drop due to less volume in the arteries. The body’s ability to transport oxygen to tissues begins to weaken; at this point, the victim is pale and may be very agitated and confused. Heartbeat is usually very rapid (over 120 beats per minute) and respirations reach 30-40 per minute in a desperate attempt to maintain oxygenation.
CLASS IV: Over 4 pints (more than 2 liters): Patient is now very pale; confusion becomes lethargy, leading to unconsciousness. The pulse is very rapid (over 140 beats per minute) and thready. After a period of continued blood loss, the blood pressure drops further. The heart rate and respirations begin to drop as the body loses the oxygenation battle. The circulatory system eventually collapses, a condition known as “hypovolemic shock.” This casualty is in serious danger without major intervention.
HOW TO STOP BLEEDING: 18 PRINCIPLES OF HEMORRHAGE CONTROL
Understanding hemorrhage and the proper use of tourniquets is necessary to be an effective off-grid medic. There are a number of principles that must be considered:
1) Know the difference between arterial and venous bleeding. Arterial blood is oxygen-rich, giving it a bright red color. It tends to spurt vigorously from the wound in time with the pulse. Venous blood is oxygen-poor and is much darker. It tends to flow more steadily. Arterial bleeding is under more pressure than venous and is, therefore, harder to stop.
2) Using your hands to apply direct pressure on the extremity will staunch the majority of cases of mild-moderate bleeding, but there are circumstances where it’s obvious you’re dealing with a life-threatening injury. In these cases, using a tourniquet immediately is usually the right move. The likelihood of survival is much higher when a tourniquet is applied before the victim has gone into shock. from blood loss.
That doesn’t mean applying pressure is useless. Upon first encountering a victim, put gloves on, if possible, and use a cloth, dressing, or other barrier to press on the area. You might be successful at stopping mild-moderate bleeding. If so, continue pressure for at least ten minutes and call for help asap, if it exists.
3) To access supplies like gloves, dressings, and tourniquets, your hands must be free. This is difficult where you’re pressing on a bleeding wound. A knee may be applied over the bleeding area to place pressure long enough to access a tourniquet, bandages, and other supplies.
4) Be aware that standard limb tourniquets are not meant for groin/hip, torso, or armpit/shoulder bleeds. Those require special devices known as “junctional tourniquets”.
5) Effective tourniquet use on extremities depends on knowing the full extent of the bleeding injury. Using shears to fully expose the limb will allow a rapid but thorough investigation of the source and extent of the hemorrhage. Place the casualty in the position most convenient for visualization. Often, this will be the “shock” position: Supine with the leg raised 12 inches or so above the heart.
6) Tourniquets are best placed on bare skin. In hostile encounters, however, bleeding may be especially severe or the medic may be under heavy fire. When you don’t have the time to cut away clothing and perform a thorough evaluation, place a tourniquet as high and tight as possible on the extremity over the clothing. If there are foreign objects or projectiles embedded in the wound, leave them in place; they might stem the bleeding. Pressure can be applied by packing alongside the object on both sides.
7) Elevation of a bleeding limb above the level of the heart may make it more difficult for the heart to pump blood out of the body, but it’s unlikely to stop bleeding altogether without direct pressure. As such, using “pressure points” away from the wound has been and is still recommended by some sources. Compressing “pressure points,” however, rarely stops heavy bleeding for two reasons: 1) finding the right spot to apply pressure may be difficult for the untrained and 2) limbs are supplied with blood by more than one artery.
 CAT tourniquet placed “high and tight”
CAT tourniquet placed “high and tight”
8) Apply the tourniquet a good 2-3 inches above the hemorrhagic wound. Why not directly on the bleed? When an artery is severed, it tends to retract back towards the torso. Avoid placing the tourniquet directly over a joint, however. Application over the nerves in joints like the knee, ankle, or elbow may result in significant damage. Go higher instead.
9) Tourniquet pressure against one bone is superior to pressure against two. In the forearm and lower leg, bleeding can occur between the radius and ulna or the tibia and fibula. Pressure against the humerus in the upper arm or femur in the upper leg will be more effective in controlling hemorrhage.

10) In most cases, deep bleeds will require packing of the open wound to reach bleeding vessels. If bleeding continues, standard dressings should remain in place; firmly pack new dressings on top of the old ones. If the wound bleeds through subsequent bandaging, consider the use of hemostatic-type dressings like Quikclot, ChitoSam or Celox. To be effective, these products must be in direct contact with the bleeding vessel. In this situation, first remove the plain gauze packing before inserting the new hemostatic gauze and then apply direct firm pressure for at least three minutes.
11) Beware of “pressure loss”. Pressure loss refers to the loss of tension (due to a decrease in tissue volume from stoppage of blood flow) under the tourniquet that occurs after the initial minute or two of placement. The tourniquet may loosen enough to allow a re-bleed. One of the benefits of sturdy elastic tourniquets like the SWAT tourniquet, that is, if it’s applied properly, is that it maintains a steady pressure underneath and prevents pressure loss from occurring.
 Two tourniquets placed one above the other
Two tourniquets placed one above the other
12) The first tourniquet may not stop the bleeding; a second one may be necessary and should be part of every medical kit. Place the second directly above the first (closer to the heart, see image).
13) Apply firm pressure when cinching the tourniquet and twisting the windlass. If the victim is not experiencing pain when you do this, you’re not applying enough pressure. It’s probably a good idea to warn them: “This is gonna hurt”. If the tourniquet is tight enough the bleeding and any pulse beyond it (farther from the heart) should both disappear. Traumatic amputations are an exception: some oozing from the bone marrow of stump may occur despite proper tourniquet placement.
14) The time of application should always be documented with a permanent marker in a clearly visible location. With regards to the military style CAT tourniquet, there is a space provided on the windlass strap itself. Luckily, placement for two hours (or even more in some studies) should pose little risk of permanent damage. In austere settings, write a “T” and time on the patient’s forehead with ashes or even blood.

15) Improvised tourniquets like a bandanna and a stick may be of help in controlling hemorrhage, but are inferior to commercially-made and military-tested items. Using a man’s tie may cause a cord-like effect so thin that it damages tissues. A tourniquet should be at least 4 centimeters (about 2 inches) wide to prevent damage to nerves underneath it. The classic leather belt tourniquet seen in movies is usually too difficult to tighten enough and can’t easily be secured in place, you will have to hold it pulled tight if used.
16) Transport of a victim with a tourniquet in place requires constant monitoring for rebleeds. Covered with blankets to avoid shock, a tourniquet (especially an improvised one) could be dislodged during the jostling that occurs during evacuation. Expose the wound area frequently to check for bleeding. Splinting (Sam splints are excellent) the extremity will help stabilize it and decrease the chance of further hemorrhage.
17) Avoid loosening or removing the tourniquet until the patient is in a controlled environment and considered stable. Repeated loosening and tightening will likely increase blood loss and worsen the condition of the victim.
 Transitioning the tourniquet; compression dressing in place
Transitioning the tourniquet; compression dressing in place
18) If it’s clear that help is not on the way and that you are the highest medical asset left, you will need to transition the casualty off the tourniquet. If possible, aim to transition to hemostatic gauze covered with a pressure dressing before the 2-hour mark. If a hemostatic gauze and pressure dressing have already been applied you may slowly loosen the tourniquet while observing for bleeding that restarts.
If no hemostatic gauze has been applied, follow these directions to safely remove a tourniquet:
- Remove old plain gauze.
- Apply hemostatic gauze packed firmly inside the wound, toward the injured vessel.
- Cover with a pressure bandage, like an Emergency Bandage (aka Israeli dressing).
- Loosen the tourniquet slightly (don’t remove it) and evaluate for recurrence of bleeding. If so, re-tighten. If not, loosen further.
- Re-evaluate when all tension has been released from the tourniquet and monitor constantly.
- Evaluate for recurrence of bleeding.
You may have some additional advice to add to the above. If so, don’t hesitate to use the contact form to write a note or comment to me.
Joe Alton MD







 General Johnston
General Johnston



 SAM Junctional Tourniquet
SAM Junctional Tourniquet Dr. Alton
Dr. Alton